Disease summary is provided courtesy of VisualDx, the visual diagnostic decision support system for health care professionals. To view more images of Cocaine Levamisole Toxicity and other visually presenting diseases and adverse drug reactions, log in to VisualDx or try it now.
Diagnosis Synopsis
- Cocaine cut with Levamisole retains the irridescent, fish-scale appearence of pure cocaine, Levamisole is a bulking agent for crack that slips through the washing process, resulting in a higher volume of crack from less pure cocaine, and Levamisole passes the bleach test (Levamisole-cut coke disolves in bleach clearly, just like pure cocaine).
- Some people still get very ill because of cocaine contaminated with levamisole. (It’s a toxic substance for de-worming animals, added by cocaine producers.) Most people doing cocaine do not react, however, people who do can have severe infections or sickness. Most crack/cocaine contains levamisole. You can’t tell if it’s there by looking at it, smelling.
Cocaine Levamisole Toxicity : Cocaine contaminated with levamisole has been detected in the United States since 2003, and the incidence of toxicity caused by this contamination has been increasing rapidly since 2008. Use of cocaine that has been adulterated with levamisole can lead to a constellation of symptoms including agranulocytosis, neutropenia, and a vasculitis-like purpuric tender skin eruption. The most common sites of purpura are the external ears and cheeks. The purpura is generally followed by skin necrosis, but resolves several weeks after cessation of cocaine use. Recurrent use of contaminated cocaine generally results in recurrent skin eruptions.
Concomitant symptoms of arthralgias, fever, and mouth pain have been reported.
The CDC estimates that approximately 70% of cocaine in the United States may be contaminated with levamisole. Toxicity induced by levamisole seems to affect all ages and both genders equally depending on cocaine use. The cocaine can be either smoked as crack cocaine or snorted. Some analyses have revealed up to 10% contamination of individual cocaine products.
Because levamisole is difficult to test for and because other treatable causes of vasculitis may be present, levamisole-induced toxicity is a diagnosis of exclusion. Several published cases have had concurrent or preceding medical histories that involve both chronic and acute infections as well as signs of chronic autoimmune disease. Other cases have had absolutely no preceding medical history.
Since neutropenia is a common presenting sign of this toxicity, bacterial or fungal infections may be presenting features of levamisole toxicity.
Look For
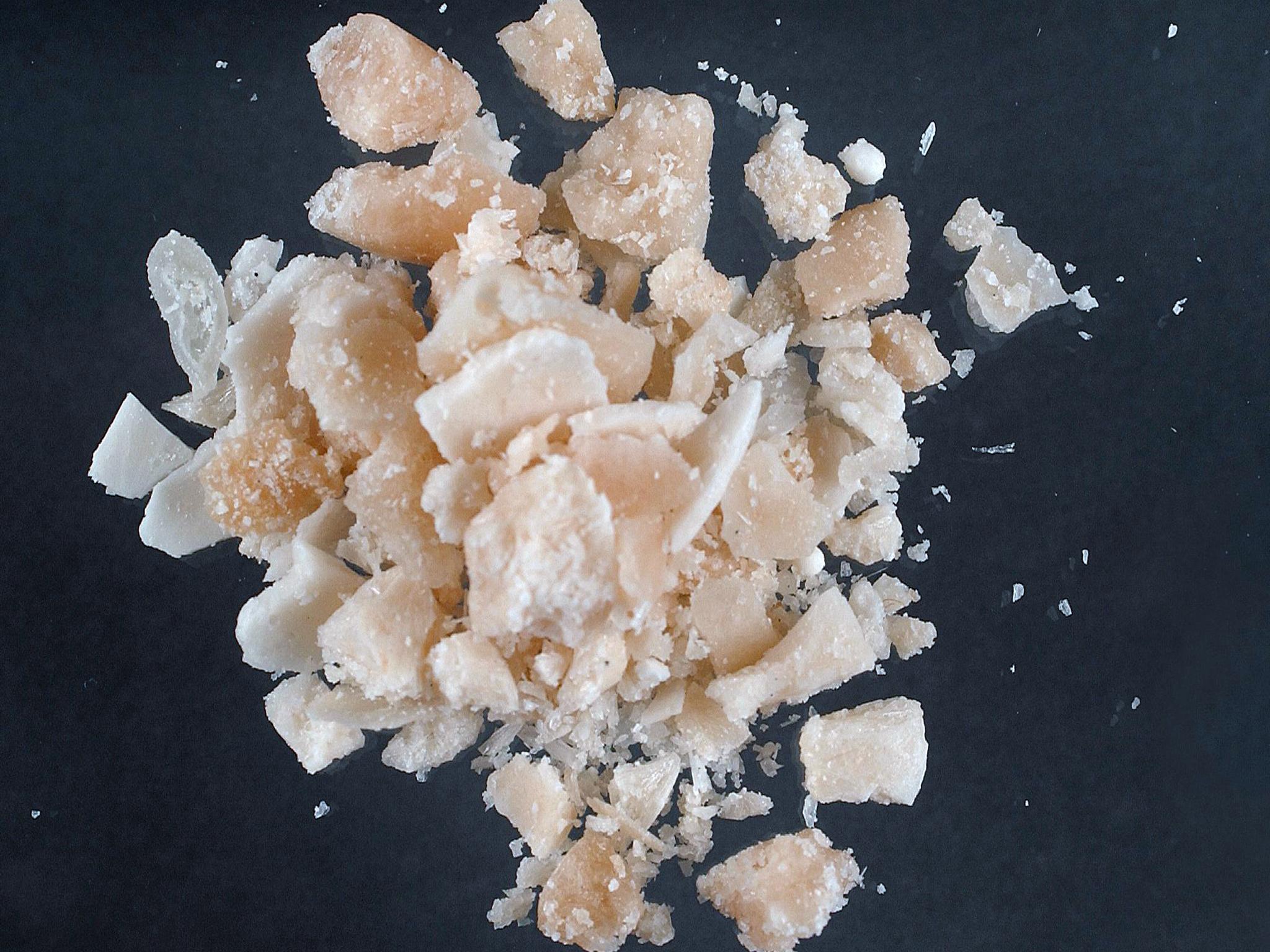
Purer forms of crack will sink in water or melt at the edges when near a flame (crack vaporizes at 90 °C, 194 °F). 1 Crack cocaine as sold on the streets may be adulterated or 'cut' with other substances mimicking the appearance of crack cocaine to increase bulk. Use of toxic adulterants such as levamisole 4 has been documented.
Somewhat tender purpuric macules and papules on the helix of the ear or the cheeks. Retiform or stellate purpura on the trunk and extremities that can progress to bullae. Very early, the purpura may be preceded by erythematous macules. Progression of the purpura to necrosis and crusting eschars is common before resolution.
Dark Skin Patient Considerations
In dark-skinned individuals, the rash may present with deep red to brown or purple macules and papules. Purpura is difficult to detect in extremely dark skin.

Diagnostic Pearls
Neutropenia is a common laboratory finding. The combination of neutropenia in a patient with purpura of the ears and a urine toxicology screen positive for cocaine should suggest levamisole-induced vasculitis. Levamisole testing of serum or urine is difficult and unreliable.
Multiple autoimmune serological markers can be positive including anti-dsDNA, ANCAs, platelet factor IV antibody, lupus anticoagulant, Russell viper venom time, elevated PTT, and anticardiolipin IgM. Careful consultation with rheumatology to consider autoimmune diseases is recommended.
Differential Diagnosis & Pitfalls
The differential diagnosis for cocaine levamisole toxicity includes many of the same diagnoses as for leukocytoclastic vasculitis (LCV) or drug toxicities. Secondary causes of LCV such as infection, medication reactions, neoplasms, and autoimmune connective tissue disorders should be sought out.
- Cryoglobulinemia – check for serum IgM and IgG cryoglobulins, HCV infection.
- Cryofibrinogenemia
- Bacterial sepsis
- Coumadin necrosis
- Heparin necrosis
- Purpura fulminans
- Acute meningococcemia – the patient is usually systemically ill, but since cocaine use may complicate the neurologic exam, this diagnosis should be considered carefully.
- Calciphylaxis
- Vasculitis secondary to viral infections such as hepatitis A, B, C, VZV, parvovirus B19, and CMV, or to medications.
- Arthropod bites
- Erythema multiforme minor (EM) – characteristic findings on histology will assist in differentiating EM from LCV. Systemic involvement is rare.
- Toxic epidermal necrolysis (TEN) – usually larger areas of skin are involved with more skin pain and resulting bullae.
- Frostbite or chilblains (perniosis) – history of recent cold exposure.
- Microscopic polyangiitis is ANCA positive and has palpable purpura and constitutional symptoms; look for evidence of pulmonary and renal involvement.
- Wegener's granulomatosis is ANCA positive and has necrotizing granulomatous inflammation of the upper and lower respiratory tracts, glomerulonephritis.
- Churg-Strauss syndrome is ANCA positive and is associated with eosinophilia and asthma.
- Polyarteritis nodosa – medium vessel vasculitis with subcutaneous nodules, livedo reticularis, ulcers, and gangrene as cutaneous manifestations.
- Immune thrombocytopenic purpura – look for isolated thrombocytopenia.

Sometimes non-vasculitic purpura on the lower extremities may be palpable such as those seen in the following:
- Over-anticoagulation with Coumadin (warfarin) or heparin
- Early disseminated intravascular coagulation
Best Tests
Cocaine levamisole toxicity is a diagnosis of exclusion and depends heavily on the history. Although very suggestive, the use of cocaine before a characteristic purpuric eruption does not necessarily implicate this drug or contamination with levamisole. It is critical to identify other treatable causes of vasculitis such as infection or autoimmune disease. It is also important to evaluate and identify any internal organ involvement.
A skin biopsy will be helpful to rule out other diseases but will not implicate cocaine or levamisole directly. Fibrin thrombi are commonly seen in the vessels, but all features of leukocytoclastic vasculitis may not be present.
Laboratory studies:
- Urine toxicology to detect cocaine use
- Liver function tests
- CBC with differential (neutropenia is a common associated finding; also look for the presence of leukocytosis, eosinophilia, and atypical lymphocytes to indicate ongoing infection or leukemia)
- Urinalysis and renal function tests
Lumbar puncture or imaging studies can be ordered to rule out other causes of vasculitis or altered mental status if localizing symptoms are present.
A skin biopsy will likely be helpful, but this diagnosis depends on ruling out other causes of vasculitis.
Management Pearls
Consultations may be needed with dermatology, critical care, infectious disease, and rheumatology. Depending on the level of cocaine abuse or the use of other addictive drugs, psychiatry may need to be consulted during withdrawal.
Elevated serological markers tend to resolve after 2-10 months.
When patients are severely neutropenic, care should be taken to monitor for concurrent bacterial and fungal infections.
Levamisole Buy

Therapy
Levamisole Fish Dosage
Use of contaminated cocaine must be stopped immediately. Management is generally supportive. Many patients will recover spontaneously, although sometimes slowly. Optimize supportive care for any specific complications or wound care.
Authors
Art Papier MD, Noah Craft MD
Comments are closed.